Background: Abatacept (Abata, CTLA4 Ig), has been explored for the past 3 decades for blockade of CD28-B7 costimulation pathway in organ transplantation. One of the disadvantages of Abata has been its sparing effect on natural killer (NK) cells, resulting in NK-mediated rejection in preclinical models. However, we explored this caveat of abatacept to augment NK cell mediated anti-leukemia effect without invoking T cell mediated GVHD, where unmodified donor lymphocyte infusions (DLI) were administered 6 hours following administration of abatacept in-vivo (Abata-DLI) to patients with advanced malignancies undergoing haploidentical (Haplo)-HCT on days +7, +21 and +35. An early and rapid proliferation of mature NK cells was observed, which correlated with an improved relapse-free survival, without an increase in GVHD. To explore the mechanistic pathway behind this phenomenon, we studied the effect of Abata on cytotoxicity as well as cytokine profile of NK cells both in-vitro as well as in-vivo (CTRI:REF/2021/08/046552).
Methods: NK cells and monocytes were isolated from PBMC of healthy donors. NK cells ± monocytes, were incubated with IL2, IL15 and IL12/15/18 with or without Abata for 72 hours and 7 days. They were assessed for cytotoxicity and IFN-g and perforin expression against K562 cell lines at effector: target (E:T) ratio of 5:1 and 1:1 . In HCT recipients, samples were obtained at day +20 (baseline), +30, +45, +60, and 6, 12 and 18 months. The samples were cryopreserved and both cytotoxicity and cytokine assays were carried out in batches after thawing. Cytokine profile was analysed in total NK cells and in NKG2A+ and NKG2C+ subsets.
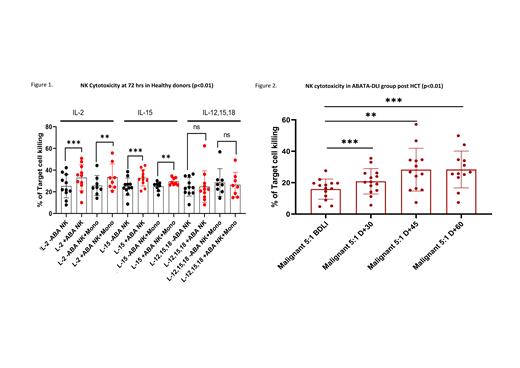
Results: The study was carried out on 11 healthy donors and 20 haplo-HCT recipients (15 with malignant diseases receiving Abata-DLI and 5 with non-malignant diseases receiving Abata without DLI). NK cells from healthy donors showed significant increase in cytotoxicity at 72 hours in presence of Abata with IL2 and IL15 (Figure1, p<0.01) at E:T ratio of 5:1 as well as 1:1 at both 72 hours as well as 7 days, but not with IL12/15/18. The effect was independent of monocytes. Perforin tended to be upregulated at both 72 hours and 7 days with Abata and IL15.
In patients receiving Abata-DLI, cytotoxicity of NK cells was significantly increased at all time points compared to baseline at E:T ratio of 5:1 and 1:1 (Fig 2, P < 0.01). NK-cytotoxicity was significantly higher than the corresponding donor samples at days +45 and +60 (p<0.05). This was particularly so in 11 patients without any event compared to 4 patients with relapse/GVHD. To evaluate if Abata-DLI had greater impact on NK-cytotoxicity, the data was compared with 5 patients who received Abata alone. This showed significantly greater cytotoxicity at days +45 and +60 in the Abata-DLI group, which was more pronounced, when only those without events were analysed from the Abata-DLI group (p<0.01).
There was no significant change in cytokine profile in those receiving Abata alone, but in Abata-DLI group, IFN-g was significantly upregulated in the NKG2C+ subset at day +60 at 1:1 ratio. Perforin expression was significantly higher at days+45 and +60 at both 5:1 and 1:1 in the Abata-DLI cohort, for both NKG2C+ and NKG2A+ subsets. In the Abata-DLI group NKG2C+ subset showed significantly higher IFN-g at days+45 and +60 and upregulation of perforin at all time points. 3 patients transplanted with active leukemia, assessed beyond day +60, showed greater cytotoxicity compared to the corresponding donors at 6-18 months.
Conclusion: In this study, Abata was shown to increase cytotoxicity of NK cells, independent of monocytes, in the presence of IL2 and IL15, but not with IL12/15/18. This was observed at both high as well as low E:T ratios, with significant upregulation of perforin. In Haplo-HCT with Abata-DLI, there was marked increase in NK-cytotoxicity with upregulation of both IFN-g and Perforin, when compared to baseline as well as in comparison to those receiving Abata without DLI. Our findings suggest that Abatacept directly augments NK-cytotoxicity and provides rationale for exploring Abata-augmented NK cell therapy as a novel approach to augment NK-mediated GVL effect without invoking T cell mediated GVHD
OffLabel Disclosure:
Savani:Takeda Development Center Americas, Inc. (TDCA): Current Employment.
Abatacept Abatacept binds to CD80 and CD86 on antigen-presenting cells and prevents binding of CD28 receptor on T cells to these ligands, resulting in abrogation of the primary costimulation pathway of T cells. This has been approved in MUD or MMUD transplantation recently. It is being investigated as an agent to augment NK cell mediated anti-leukemia effect without invoking T cell mediated GVHD

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal